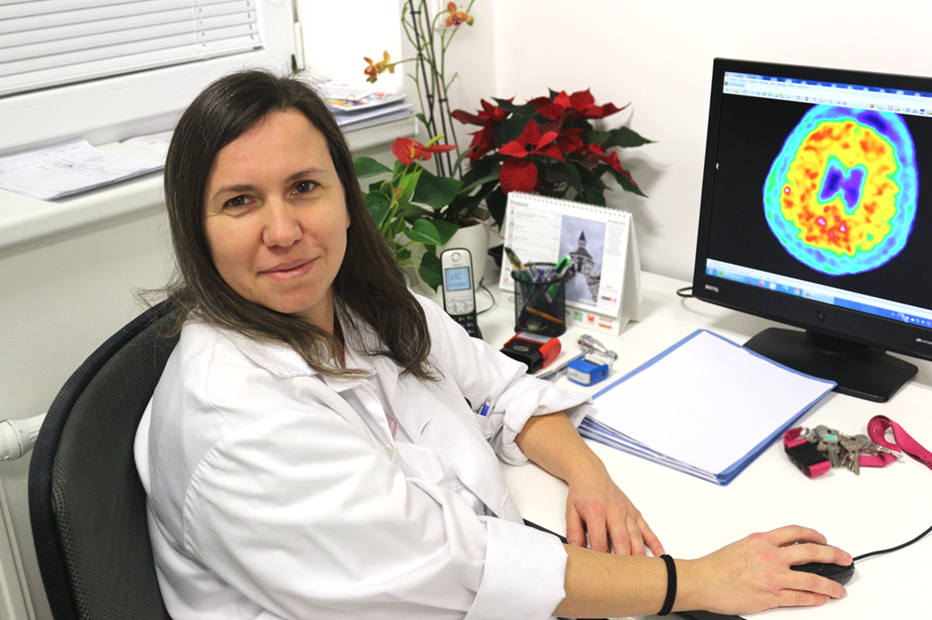
Changes in the gut may contribute to brain disease, says neurologist and scientist Lenka Krajčovičová
Neurologist Lenka Krajčovičová, in addition to diagnosing and treating patients with neurodegenerative diseases at the Center for Cognitive Disorders at the First Department of Neurology of St. Anne’s University Hospital in Brno, is also involved in research on Alzheimer’s and Parkinson’s disease at ICRC and NEUR-IN. She has now embarked on studying the gut microbiome and its impact on the development of these diseases. How are our gut and brain connected, and how does the health of one organ affect the condition of the other?
What Does the Term Gut Microbiome Encompass?
It refers to the collection of microorganisms that inhabit the intestinal lining. This includes all microorganisms—not just bacteria but also viruses, yeasts, and other types of microbes. The term microbiome also encompasses their environment, such as the substances these organisms produce and essentially the entire ecosystem associated with them.
When Did the Discussion About the Gut’s Influence on the Brain Begin? When Did It Become a Subject of Scientific Study?
This connection has been known for quite some time, but research into the microbiome in relation to neurodegenerative diseases has gained momentum only in the last ten years.
Why Did the Study of the Gut Microbiome Catch Your Attention as a Neurologist?
Originally, I became interested in this topic in relation to Parkinson’s disease. It has been known for some time that this disease is somehow linked to the digestive system. Before Parkinson’s patients develop their first symptoms and come to our clinic, they often experience gastrointestinal issues—typically constipation—which then continues throughout the course of the disease. This led researchers to investigate the relationship between the gut and the disease.
Detailed gut analyses revealed pathological changes—first, the same protein responsible for neurodegeneration in the brain, synuclein, was found in the intestines of patients. Additionally, the gut may experience a decrease in neurotransmitters, which are substances that mediate nerve signaling. This led to the hypothesis that the microbial composition of the gut might play a role. It is well known that microbiome imbalances are linked to other diseases, so it is reasonable to hypothesize that these changes might contribute to the development of neurodegenerative diseases.
Does This Mean That the Gut Is Not Just an Indicator of Disease—A Place Where Early Symptoms Can Be Observed Before They Appear in the Brain—But a Cause of the Disease Itself?
The communication is bidirectional. Yes, changes in the gut can affect brain function and contribute to the development of these diseases, but the brain can also influence the gut. This connection is known as the gut-brain axis. It happens either through direct nerve communication—the brain can regulate gut motility via the vagus nerve—or through neural endings in the gut that send signaling molecules to the brain.
There is also an indirect pathway: various substances, primarily nutrients, enter the bloodstream from the gut. Many cells in the gut, whether they belong to the organ itself or to the microorganisms living in it, release signaling molecules that serve to inform the brain. A common example is the signaling that occurs after eating, letting the brain know that the body is full and no longer needs to consume more food.
Gut microbiome helps control intestinal digestion and the immune system




